
Variations in Peripheral Hematological Parameters as a Diagnostic Biomarker of HBV Infection
- Applied Molecular Biology and Biomedicine Lab, Department of Zoology, University of Narowal, Narowal, Pakistan
- Molecular Medicine and Cancer Therapeutics Lab, Department of Zoology, Faculty of Sciences & Technology, University of Central Punjab, Lahore, Pakistan
- University of Veterinary and Animal Sciences (UVAS), Lahore, Pakistan
- Department of Zoology, University of Okara, Punjab, Pakistan
- Cell & Molecular Biology Lab, Institute of Zoology, University of the Punjab, Lahore, Pakistan
Abstract
Background: Hepatitis B virus (HBV) is a major global health concern that can cause both acute and chronic liver infection in humans and cause hepatitis B. The main purpose of our investigation was to show the changes in peripheral hematological parameters as a diagnostic biomarker in hepatitis B patients due to HBV compared to healthy controls.
Methods: Blood samples from HBV patients already diagnosed by clinicians and healthy subjects were collected from various hospitals in Punjab. The complete blood count (CBC) test and t test were applied to these samples.
Result: The hemoglobin (HB), hematopoietic cell transplantation (HCT), mean corpuscular hemoglobin concentration (MCHC), mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), and neutrophil/lymphocyte ratio (NLR) of patients and controls showed great differences. The white blood cells (WBCs), red blood cells (RBCs), platelets, neutrophils, lymphocytes, monocytes, and eosinophils in hepatitis B patients showed no association.
Conclusion: Our primary results indicate a promising biomarker to monitor HBV infection by using information from hematological parameters. Further large cohort investigations are required for more accurate results.
Introduction
The liver is a vital organ in the human body that performs a variety of activities, including metabolism, immunity, digestion, detoxification and vitamin storage1 . Unlike other solid organs, the liver can repair itself2. Every year, approximately 2 million individuals die from liver disease, 1 million from complications of cirrhosis, and 1 million from viral hepatitis and hepatocellular carcinoma3. When the liver is inflamed or injured, it may lose its ability to function4. The word "hepatitis" means "liver inflammation". Hepatitis can be caused by excessive use of alcohol, drugs, pollutants, and certain illnesses. On the other hand, hepatitis is primarily caused by viruses5. More than 350 million individuals are infected with HBV, which was identified in 1966. Hepatitis B is the major cause of chronic hepatitis, cirrhosis, and hepatocellular cancer, with 1 million people dying each year6.
HBV is a member of the hepadnavirus family, and the viral genome within the HBV particle is a circular, partly double-stranded, relaxed circular DNA molecule7. Infection with HBV is a major global health concern that can cause both acute and chronic infections in humans. HBV is transferred through blood vessels, skin, or mucous membranes by infected blood or other bodily fluids. The virus can be found in all human bodily fluids, with the viral concentration in fluids being greatest in blood or serous exudates and relatively low in saliva, sperm, and vaginal secretions8.
Pakistan is extremely endemic for HBV9, with nine million persons affected and the infection rate steadily increasing. HBV carriers account for 7-9 million people in Pakistan, with a carrier prevalence of 3-5%10. Punjab, along with Sindh's interior and war-affected areas, was Pakistan's most contaminated region11. Balochistan has the highest intraprovincial prevalence of hepatitis B (4.3%), followed by Sindh (2.5%), Punjab (2.4%), and Khyber Pakhtunkhwa (1.3%). Punjab Province has a 2.4% total HBsAg prevalence. Vehari, Okara, Jhang, Islamabad, Attock, Rahim Yar Khan, Mandi Bahauddin, Gujranwala, and Mianwali districts of Punjab Province have a high frequency of HBV and HCV. Hepatitis virus may be more common in those who live in polluted settings12.
The goal of this study was to examine the inflammatory aspects of complete blood counts (CBCs) in HBV patients, to determine which promising biomarkers differentiate patients and healthy subjects and to discover a cheap, quick, and simple biomarker to monitor HBV infection in Pakistan.
Methods
Subject Selection
The subjects were recruited between August 2019 and January 2022 at various hospitals in Narowal. HIV-positive subjects diagnosed by physicians were included in this study.
Blood Sampling
A total of 200 healthy and patient blood samples were collected. After collection, a CBC test was performed.
Selection of Hematological Parameters
The hematological parameters in this study included HB, HCT, MCHC, MCV, MCH, NLR, RBCs, WBCs, platelets, neutrophils, lymphocytes, monocytes, and eosinophils.
Statistical Analysis
Student’s t test was applied using IBM SPSS version 21 for the statistical analysis of the selected parameters of infected and healthy patients to check the similarities and differences in numerous blood parameters.
Results
Population Characteristics
In our study cohort, the male to female ratio was maintained in patients and healthy subjects, as shown in Figure 1, Figure 2.
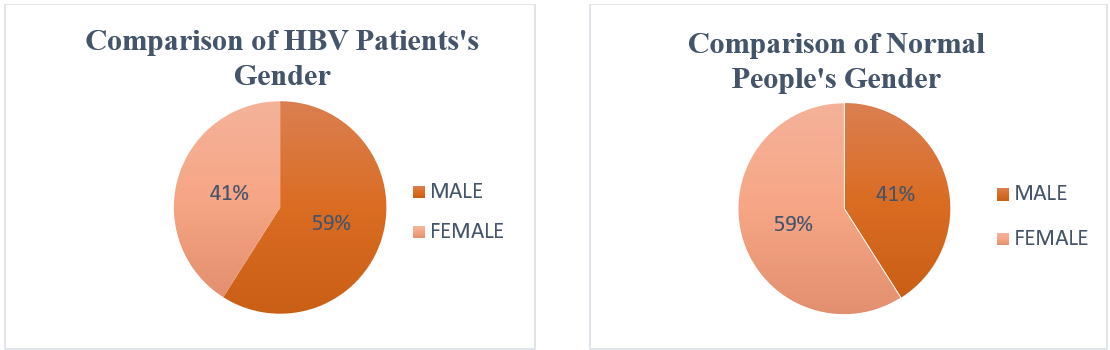
Pie chart shows the male and female individuals of HBV Patients group.
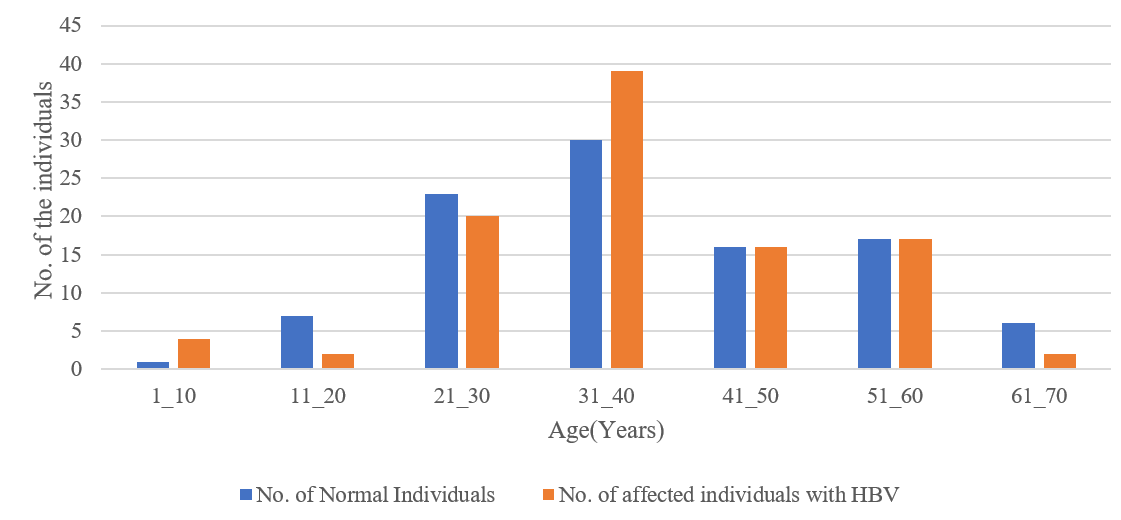
Age bar chart shows the number of HBV and Normal individuals with different age (Years). Blue represents Normal individuals and Orange represent Affected individuals.
The characteristics of population under study
|
Population |
Male % |
Female % |
Total % |
|---|---|---|---|
|
HBV Affected group |
59 |
41 |
100 |
|
HBV Control group |
41 |
59 |
100 |

Comparison of various hematological parameters in HBV cases (red) and normal subjects (green). There was a significant difference in (a) HB, (b) HCT, (g) MCHC, (h) MCV and (m) NLR. Whereas, (b) WBCs, (c) RBCs, (d) lymphocytes, (f) MCH, (i) Platelet count, (j) eosinophil, (k) monocytes and (l) neutrophils showed no significance difference between the groups.
Evaluation of hematological parameters
The outcome of the analysis of our cohort (
Discussion
In our studies, there was a significant change in HB, WBCs, HCT, MCV, MCH and MCHC in normal and hepatitis B patients, while there was a slight difference in platelets, monocytes and eosinophils, and there was no difference in RBCs, lymphocytes, or neutrophils.
In hepatitis B patients, HB, HCT, MCV, MCH, monocytes and eosinophils were decreased compared to those in control individuals, while WBCs, MCHC, NLR and platelets were increased. Regarding the remaining parameters, RBCs, lymphocytes and neutrophils showed no change.
When patients with HBsAg were receiving intense immunosuppression or chemotherapy, hepatitis caused by HBV reactivation was a significant cause of morbidity and mortality13. Our results show a highly significant difference in HB in HBV patients. The level of HB decreased in HBV patients because viral infections, including hepatitis viruses, frequently cause anemia, which is a common hematological complication14. In contrast to these studies, in our study, HB was decreased in Hepatitis B patients.
In our study, there was no significant change in RBCs of normal and hepatitis B patients. Red blood cells are destroyed before they reach their normal 120-day life span in a condition known as hemolytic anemia, which causes jaundice and hemoglobinuria from free hemoglobin15. Rarely, especially following HBV infection, can acute hepatitis present with hemolytic anemia as an extrahepatic symptom16. Another type of anemia caused by a significant decrease in erythroid precursors in the bone marrow is called HBV-related pure red cell aplasia (PRCA)17.
Our results show a significant difference in HCT in HBV patients the level of HCT decreases compared to that in normal individuals because hematologic and oncologic conditions are now commonly treated with HCT18. In regions where HBV infection is common, such as Southeast Asia, HCT may be worsened by HBV-related morbidity and mortality. More than 10% of Asian Chinese patients undergoing HCT have been observed to be HBsAg positive on average. After HCT, HBV reactivation is primarily linked to hepatic problems caused by HBV infection13.
Hu, Lou et al. discovered that chronic severe hepatitis B (CSHB) and chronic hepatitis B (CHB) patients had MPVs that were considerably greater than those of HCs and acute hepatitis B (AHB) patients. Additionally, among all the patients, the CSHB patients had the highest MPVs. Because 90–95% of adult patients have spontaneously self-limited acute hepatitis without overt symptoms, it is widely recognized that AHB patients are less frequently observed in the clinical context. These individuals frequently go through a convalescence phase after a brief acute phase before seeing a doctor. As a result, there was no discernible difference in MPV between HCs and AHB patients. It is hypothesized that these variations have a significant role in the development of the disease and could be used to identify patients with HBV infection. Patients with HBV infection had a considerably higher MPV infection rate19. In a previous experiment, the platelet volume increased in HBV patients, and in our studies, the mean platelet volume also increased. It has been established that platelets and HBV interact closely. HBV can directly infect bone marrow, suppress platelet synthesis, and speed up platelet breakdown by stimulating the immune system and monocyte-macrophage system20. According to severity, MPV values are significantly elevated in HBV-infected patients and can be considered independent predictors of hepatic fibrosis21.
According to a study, individuals with chronic liver failure had considerably greater MCVs than healthy controls (HCs). The study showed that MCV was related to the degree of liver impairment and may be a predictor of death in HBV-related patients in cross-sectional research22.
Anemia may be a frequent complication in cirrhosis that is linked to a poor prognosis. Ahmad et al. stated that there were no significant changes in RBC concentration23. Our findings are in agreement with the findings of Ahmad because in our study, there was also no significant change in RBCs of normal or affected individuals.
Cai and Wang et al. found that patients who had liver failure had WBC counts that were considerably higher. Additionally, patients with acute-on-chronic liver failure (ACLF) had significantly lower lymphocyte counts and significantly higher circulating neutrophil and monocyte counts than patients in the cirrhosis (LC) and chronic hepatitis B (CHB) groups24. Similarly, in our study, WBCs were also increased in hepatitis B patients compared to normal individuals.
Zhang, Sun examined the capacity of the blood NLR to predict 1-month mortality in HBV-related decompensated cirrhosis (HBV-DeCi) patients, a straightforward marker that represents the degree of inflammation. The two crucial things were discovered. First, an increased frequency of liver-related problems, such as hepatorenal syndrome (HRS), was connected with a higher NLR. Second, an elevated NLR level can be a reliable predictor of mortality in HBV patients, and the risk of mortality increases with NLR25. Our study correlates with this study because in our study, NLR also increased in hepatitis B patients.
Zhang et al. found that neutrophil counts in the peripheral blood of CHB patients were significantly lower than those in healthy controls and that these neutrophil counts corresponded with the stage of the disease in CHB patients. The buildup of hepatic neutrophils was linked to liver damage26. In contrast to their study, our study shows that there is no difference in neutrophils of control and HBV-infected individuals.
Zhang also examined peripheral monocytes from CHB patients and unaffected individuals. The absolute numbers of these cells were higher in CHB patients26. In our study, the level of monocytes was slightly decreased in hepatitis B patients compared to normal individuals.
Conclusions
In our examination, it was investigated whether different peripheral hematological parameters might help to diagnose individuals suffering from hepatitis B. Our study shows that there is a significant change in HB, WBCs, HCT, MCV, MCH and MCHC in normal and hepatitis B patients, while there is a slight difference in platelets, monocytes and eosinophils, and there is no difference in RBCs, lymphocytes, and neutrophils. Although our primary results indicate a promising biomarker for the diagnosis of HBV, further large cohort investigations are required for more accuracy.
Abbreviations
CBC: Complete Blood Count, MCHC: Mean Corpuscular Hemoglobin Concentration, HCT: Hematopoietic Cell Transplantation, HB: Hemoglobin, HBV: Hepatitis B Virus, MCH: Mean Corpuscular Hemoglobin, MCV: Mean Corpuscular Volume, NLR: Neutrophil/Lymphocyte Ratio, RBCs: Red Blood Cells, WBCs: White Blood Cells
Acknowledgments
The authors are thankful to the Vice Chancellors of University of Narowal, Narowal, Pakistan, University of Okara, Punjab, Pakistan, and University of the Punjab, Lahore, Pakistan for providing the platform for the accomplishment of this study.
Author’s contributions
Rasheed H, Habiba U and Aman S performed the experimentation. Khawar M B and Afzal A analyzed and tabulated the data. Shah S S, Hamid S E and Rafiq M wrote the final manuscript. Azam F, Mehmood R and Afzal N revised the final manuscript. Afzal A edited the manuscript. Khawar M B, Abbasi M H and Sheikh N put forward the idea and approved the final manuscript. All authors have read and approved the final manuscript.
Funding
None.
Availability of data and materials
Data and materials used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
This study was conducted in accordance with the amended Declaration of Helsinki. The institutional review board approved the study, and all participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.

