A review on etiopathology and outcome in pre-eclampsia
- Department of Anatomy, Government Medical College, Nizamabad, Telangana, India
Abstract
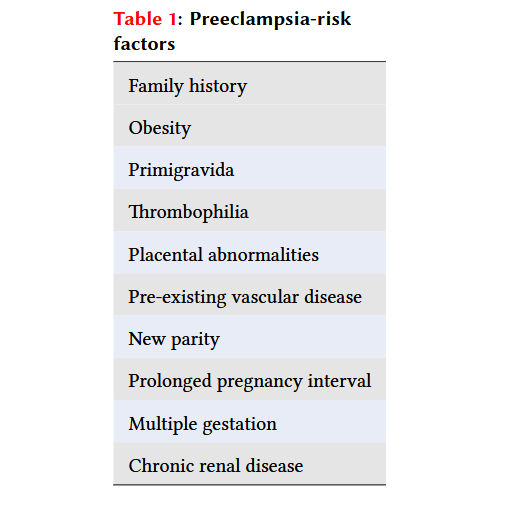
Preeclampsia is a major cause of premature birth, intrauterine growth restriction (IUGR), maternal and fetal morbidity, perinatal mortality, and accounts for 15–20% of maternal mortality cases. It is categorized as mild, moderate, or severe. Risk factors include obesity, primigravida status, placental abnormalities, multiple gestation, chronic renal disease, and family history, among other factors. Endothelial dysfunction and vasospasm are recognized as the underlying pathologies contributing to systemic vascular involvement. According to current research, vascular endothelial dysfunction arises from a deficiency in vascular endothelial growth factor (VEGF). This VEGF deficiency in preeclampsia is linked to elevated levels of soluble fms-like tyrosine kinase-1 (sFlt1), which antagonizes VEGF signaling. Placental ischemia and hypoxia represent the final pathway in the pathophysiology of preeclampsia, triggering the release of vasoactive substances into maternal circulation and resulting in endothelial dysfunction that manifests as clinical signs and symptoms.
Introduction
Preeclampsia (PE) is characterized by elevated blood pressure and excessive levels of protein in the urine that begin at 20 weeks of gestation. Its overall prevalence rate is 5-8%, which is a major cause of Intrauterine Growth Restriction (IUGR), preterm birth, morbidity, perinatal fatalities, and 15–20% of maternal mortality 1, 2. PE predicts a greater risk of cardiovascular and metabolic disorders as age advances, which may necessitate lifestyle counseling and intervention. Preeclampsia remains the most common cause of maternal and perinatal death and morbidity 3, 4. If blood pressure and proteinuria rise significantly, or if there are indications of end-organ damage, it is termed severe. There are no well-established primary prevention strategies. Despite evidence-based management, prevention measures, and screening tools are limited to symptomatic treatment, and delivery remains the only cure 5. Despite extensive research, the etiology remains unclear. There has been no significant change in preeclampsia treatment in over 50 years 6.
Classification of PE
For management purposes, PE is categorized based on blood pressure (BP) levels. Proteinuria, on the other hand, is more important than blood pressure in predicting fetal outcome. Classification by Yorkshire series based on severity forms basis for PE classification.
-
Mild: A prolonged rise in BP greater than 140/90 mm Hg but below 160- or 110-mm Hg diastolic along with proteinuria of 0.3 g /24 hrs.
-
Moderate: BP of 150/100 mm Hg with proteinuria of 0.3 g /24 hrs.
-
Severe: BP of 160/110 mm Hg or more with proteinuria of 1 g/ litre
7 ,8 ,9 .
Causes of PE
Risk factors are basically classified into immunological and genetic9, 10 shown in
Preeclampsia-risk factors
|
Family history |
|
Obesity |
|
Primigravida |
|
Thrombophilia |
|
Placental abnormalities |
|
Pre-existing vascular disease |
|
New parity |
|
Prolonged pregnancy interval |
|
Multiple gestation |
|
Chronic renal disease |
Other risk factors also include vision abnormalities, shortness of breath, renal dysfunction, decreased liver function, edema and low platelet count.
Etiopathogenesis of PE
Under normal circumstances, endovascular trophoblasts penetrate the spiral arterioles of the uteroplacental bed and remodel them into large-diameter arteries with high capacitance and unrestricted blood flow11. Aberrant spiral arterial remodeling in pregnant women with a hypertensive disorder was first noticed and studied more than five decades ago 12. It has now been discovered to be the main cause of gestational hypertension, intrauterine growth restriction, and preeclampsia in pregnancies13. Atypical placentation has placental hypoperfusion as a cause as well as an outcome14, 15. In placental tissue, atherosclerosis, thrombosis, arteriosclerosis, fibrinoid necrosis, and infarction are the late pathological changes observed, which correlate with ischemia16. Endothelial dysfunction and vasospasm continue to be the underlying pathologies that affect all vessels. The development of eclampsia/preeclampsessa is independent of blood pressure levels17.
Pathophysiology
Although the primary pathology leading to preeclampsia remains unknown, the pathological changes are well-documented. Since the removal of the placenta is necessary to alleviate the symptoms, it always plays a significant role in the etiology of preeclampsia (PE) 18, 19. Placental growth factor (PlGF) and soluble fms-like tyrosine kinase-1 (sFlt-1) are two angiogenic factors thought to be involved, according to recent research. Current molecular studies suggest that a reduction in VEGF causes dysfunction of the vascular endothelium in PE. The mechanism behind the inhibition of VEGF production in PE is attributed to elevated levels of sFlt-1, a potent inhibitor of VEGF production 20, 21, 22.
In PE, endothelial dysfunction results from an antiangiogenic state mediated by soluble endoglin, associated with lower levels of PlGF and VEGF, and high levels of sFlt-1. The placenta produces large amounts of sFlt-1, but in preeclampsia, an additional source of production is the circulating mononuclear cells 23, 24. In women with PE, higher levels of circulating sFlt-1 have been reported, which may precede the onset of PE, and the levels of sFlt-1 might correlate with the severity of PE 25, 26.
A key mediator in the development of PE is sFlt-127. The link between the occurrence of PE and the adaptive immune response is inflammation28. Placental DNA released into fetal and maternal circulation plays a major role in the characteristic inflammation associated with PE 29. The link between PE and maternal infection revealed that women with periodontal disease and urinary tract infections are at an increased risk of PE30, 31, 32. Most data suggest that both maternal and paternal genes are responsible for the development of placental abnormalities and subsequent PE33. The onset of the disease is likely influenced by genetic factors 34, 35. The final pathogenesis pathways of PE include ischemia and placental hypoxia, which release vasoactive substances into maternal circulation and cause endothelial cell dysfunction, leading to the signs and symptoms of PE 36, 37.
Maternal Outcome
The rates of adverse perinatal and maternal outcomes between primigravida and multigravida pregnancies showed no significant difference 38. The most common causes of maternal death are permanent neurological sequelae due to ischemia or cerebral hemorrhage, accounting for 0-14% of maternal mortality rates39. Additionally, 2-3% of women with preeclampsia experience complications due to eclampsia, which may lead to maternal morbidity and mortality 40.
Fetal Outcome
Intrauterine growth restriction, intrauterine death, asphyxia, and prematurity are consequences based on the duration and severity of the disease and the degree of proteinuria. Belay Tolu L et al. observed a 1.7% stillbirth rate, 2.27% neonatal death rate, 12% incidence of IUGR, and an 18.2% rate of preterm birth in their study 38. Oligohydramnios and IUGR are the primary consequences in preeclampsia due to decreased placental perfusion41. Adverse perinatal events are due to the underlying pathology of the placenta. In preeclamptic mothers who deliver preterm, aberrant placental weight indicates an adverse neonatal outcome 42. Preterm delivery owing to HELLP syndrome or preeclampsia was associated with necrotizing enterocolitis requiring surgery, a lower incidence of intracerebral hemorrhage, periventricular leukomalacia, and death when compared to other causes of preterm birth after adjustment for confounding variables 43. Neonatal death and morbidity in severe preeclampsia are linked to gestational age rather than the absence or presence of the HELLP syndrome44.
Conclusion
In spite of several theories and documented mechanisms, the etiology of preeclampsia remains unclear. It is a principal cause of maternal mortality and morbidity that affects both the mother and fetus. Its etiology presents a challenge that requires thorough research to understand its complexity. Translational research is now required to demonstrate how these developing concepts might be applied to aid in early diagnosis and treatment.
Abbreviations
BP (Blood Pressure), DNA (Deoxyribonucleic acid), HELLP (Hemolysis, Elevated Liver enzymes, and Low Platelet count), IUGR (Intrauterine Growth Restriction), mm Hg (millimeters of mercury), PE (Preeclampsia), PlGF (Placental Growth Factor), sFlt-1 (Soluble fms-like tyrosine kinase-1), and VEGF (Vascular Endothelial Growth Factor).
Acknowledgments
None.
Author’s contributions
All authors significaly contributed to this work, read and approved the final manuscript.
Funding
None
Availability of data and materials
None.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.

