Lifestyle Modification Practice and Associated Factors among People with Hypertension Attending Chronic Follow-Up Units in Public Hospital in Addis Ababa, Ethiopia
- Kasim Mohammed Hussein (MPH General public health) Federal Ministry of Health, Medical Services Lead Executive Office, Specialty and Rehabilitation Services Desk officer, Ethiopia
- Maternity and Reproductive health, St. Paul’s Hospital Millennium Medical College, Addis Ababa Ethiopia
- Eka Kotebe General Hospital Addis Ababa, Ethiopia
- Federal Ministry of Health, Medical Services Lead Executive Office, Specialty and Rehabilitation Services Desk Case Team Head, Ethiopia
Abstract
Introduction: Hypertension is a major global health problem, particularly in low- and middle-income countries (LMICs), where limited resources impair optimal disease management. Despite the availability of effective pharmacotherapy, adherence to recommended lifestyle modifications remains suboptimal. The present study assessed lifestyle practices among hypertensive patients attending Eka Kotebe General Hospital, Addis Ababa, in 2023.
Methods: A facility-based cross-sectional study was conducted from 1 to 30 September 2023 at Eka Kotebe General Hospital, Addis Ababa, Ethiopia. Data were collected through face-to-face interviews using a structured questionnaire, entered into EpiInfo version 7.1, and analyzed with SPSS version 20. Binary logistic regression followed by multivariable analysis was performed to identify independent predictors of lifestyle-modification practice. Variables with a P-value < 0.05 in the multivariable model were considered statistically significant, and adjusted odds ratios (AORs) with 95 % confidence intervals (CIs) were reported.
Results: Of the distributed questionnaires, 96.7 % were completed; 51.7 % of respondents were < 65 years of age and 50.0 % were male. Overall, 165 participants (42.9 %) demonstrated good lifestyle-modification practice. Independent predictors of good practice included a monthly income > 1500 ETB (AOR = 2.5, 95 % CI: 1.3–4.7), age < 65 years (AOR = 1.9, 95 % CI: 1.2–3.1), presence of co-morbid conditions (AOR = 2.2, 95 % CI: 1.1–4.3), and good knowledge of lifestyle modification (AOR = 2.2, 95 % CI: 1.4–3.4).
Conclusions: Less than half of hypertensive patients adhered to recommended lifestyle modifications. Higher income, younger age, co-morbidity, and better knowledge were associated with good practice. Strengthening patient counseling on lifestyle modification is therefore warranted.
Introduction
Non-communicable diseases (NCDs) constitute a growing global health concern, particularly in low- and middle-income countries (LMICs), where health systems frequently struggle with limited resources, limited service availability, and shortages of trained personnel and essential medicines 1,2. Among NCDs, hypertension remains a major contributor to morbidity and mortality, affecting more than 1.28 billion adults aged 30–79 years worldwide and imposing a disproportionate burden on LMICs. Alarmingly, 46 % of individuals with hypertension are unaware of their condition, and only 21 % achieve adequate blood-pressure control 3,4,5.
Hypertension is defined as a persistent elevation in blood pressure, characterised by systolic blood pressure readings ≥140 mmHg or diastolic blood pressure readings ≥90 mmHg. Pharmacologic treatment is recommended for adults aged ≥60 years when blood pressure reaches 150/90 mmHg and for younger adults when it reaches 140/90 mmHg 6. Despite the availability of effective medications, sub-optimally controlled hypertension remains a global problem, often attributable to inadequate adherence to lifestyle modifications 7.
Lifestyle modification (LSM) is a cornerstone of hypertension prevention and management. It encompasses dietary changes (e.g., the DASH diet), regular physical activity, smoking cessation, moderation of alcohol intake, and weight management. These non-pharmacologic interventions are recommended as first-line therapy or as adjuncts to pharmacologic treatment. Sustained adherence to LSM is essential for therapeutic success and long-term blood-pressure control 7,8,9.
Nevertheless, adherence to lifestyle modification remains suboptimal—particularly in low- and middle-income countries (LMICs). In Ethiopia, investigations indicate that only 23 %–39.5 % of hypertensive patients comply with recommended lifestyle practices. Determinants of adherence include age, educational attainment, duration of diagnosis, comorbidities, and knowledge of hypertension 10; ethnicity and family history also exert influence. Reported prevalence of uncontrolled hypertension attributable to poor lifestyle adherence ranges from 11.4 % at Gondar University Hospital 9 to nearly 70 % at Zewditu Memorial Hospital 11.
Despite the well-documented benefits of lifestyle modification (LSM), Ethiopia lacks national-level data evaluating lifestyle behaviours among hypertensive patients; existing studies focus predominantly on pharmacological therapy and thereby overlook the essential contribution of lifestyle interventions. This evidence gap underscores the necessity for focused investigations to elucidate barriers to adherence and to develop culturally appropriate strategies.
Lifestyle modification represents not merely a collection of behaviours but a dynamic, patient-centred process requiring knowledge, discipline, commitment, and self-efficacy. It encompasses regular clinic visits, home blood-pressure monitoring, stress-management techniques, and education-driven empowerment. In primary-care settings, aligning patients’ lifestyles with guideline recommendations remains challenging 10,12,13,14.
Given Ethiopia’s constrained healthcare resources, promoting lifestyle modification constitutes a cost-effective approach to mitigating the burden of hypertension and its sequelae, including cardiovascular and renal diseases. Identifying adherence gaps will inform policy and facilitate programmes that foster sustainable behavioural change 15.
In summary, lifestyle modification is a critical yet underutilised component of hypertension management in Ethiopia and other LMICs. Strengthening awareness, education, and support systems for patients can enhance adherence and improve health outcomes. Future research should therefore prioritise characterising lifestyle behaviours and their impact on blood-pressure control to guide effective public-health interventions.
Methodologies
Study setting, population, and design
An institution-based cross-sectional study was conducted between 1 and 30 September 2023 at Eka Kotebe General Hospital, Yeka Sub-City, Addis Ababa, Ethiopia. Addis Ababa, the capital of Ethiopia, had an estimated population of 6.6 million in the 2007 national census. Yeka is one of the 11 sub-cities of Addis Ababa and accommodates one federal government hospital, six health centres, and several private clinics 16.
Eka Kotebe General Hospital, founded in 2009, is a public facility that provides medical and psychiatric services. Its specialised units include a diabetes clinic that also manages chronic conditions such as hypertension. The source population comprised all patients with hypertension attending follow-up care at Eka Kotebe General Hospital during the study period. The study population included hypertensive patients who had been receiving care for at least six months. Individuals with cognitive impairment or those who were critically ill at the time of data collection were excluded.
Sample size and sample procedure
The sample size was calculated using the single-population proportion formula, based on a previous Ethiopian study that reported a 52.7 % prevalence of recommended lifestyle modification among hypertensive patients 10. Assuming a 95 % confidence level, a 5 % margin of error, and an additional 5 % to compensate for non-response, the final sample size was 398 patients. Systematic random sampling was applied to recruit participants. The sampling interval (K) was computed as K = N/n, where N = 1254 (the total number of hypertensive patients attending follow-up during the study period) and n = 398 (the required sample size), yielding K ≈ 3.15, which was rounded down to 3. Therefore, every third patient was selected for inclusion in the study. The first participant was selected by lottery. Data were collected via exit interviews in the outpatient department (OPD).
Operational definition
Good Lifestyle Modification Practice: Patients who scored above the mean on all recommended lifestyle-modification practice items 6,17.
Poor Lifestyle Modification Practice: Patients who scored below the mean on all recommended lifestyle-modification practice items 6,17.
Salt Control Practice: Participants who consumed salt-free meals during both cooking and eating on at least six of seven days per week were classified as adherent to a low-salt diet 8,18.
Knowledge of Lifestyle Modifications: Knowledge was evaluated using specific questions; participants achieving scores above the mean were categorized as having adequate knowledge of the effect of lifestyle modifications on blood-pressure control 8,18.
Data collection tool and procedures
Data were collected using an interviewer-administered structured questionnaire. The questionnaire comprised four main components: socio-demographic characteristics, participants’ health profiles, personal factors (self-efficacy and knowledge), and lifestyle-modification practices. Items assessing socio-demographic characteristics, participants’ health profiles, and personal factors were developed following a review of pertinent literature 6,17,19,20. Lifestyle-modification practices were evaluated with items adapted from the Hypertension Self-Care Activity Level Effects (H-SCALE) instrument, endorsed by the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) 7 and validated in multiple studies 6,17,19,20,21,22. The self-reported H-SCALE comprises five lifestyle-modification domains—abstinence from alcohol, cessation of khat chewing, smoking avoidance, weight management, salt restriction, and physical activity—across 27 items, and demonstrates a Cronbach’s α of 0.75. Salt restriction is assessed with eight items scored 0–7, yielding a possible total score of 0–56. Smoking avoidance is measured by one item scored 0–7. Physical activity is assessed with one item scored 0–7. Weight-management practices are measured with ten items rated on a 5-point Likert scale (1 = strongly disagree to 5 = strongly agree), giving a total of 10–50. Knowledge is assessed with a dichotomous scale (1 = correct, 0 = incorrect/“don’t know”) across ten items; scores of 1–5 indicate poor knowledge, whereas 6–10 indicate good knowledge 23. Two diploma-level nurses collected the data using the pre-tested interviewer-administered questionnaire, supervised by a Bachelor-prepared nurse.
Data processing and analysis
The data were checked for completeness, edited, cleaned, and coded, then entered into Epi Info version 7.2.0.1 and exported to the Statistical Package for the Social Sciences (SPSS) version 25 for analysis. Descriptive statistics (frequencies and proportions) were generated and presented in appropriate tables and figures. Bivariate analysis was used to identify factors associated with lifestyle-modification practices. Variables with a p-value < 0.25 in the bivariate analysis were entered into the multivariable logistic regression model. Model fit was evaluated with the Hosmer–Lemeshow goodness-of-fit test (p = 0.797), and multicollinearity was assessed using the variance inflation factor (VIF = 1.26). Multivariable logistic regression was performed using the backward likelihood-ratio method to identify factors independently associated with the outcome. A p-value < 0.05 was considered statistically significant. Associations were reported as odds ratios (ORs) with 95 % confidence intervals (CIs).
Result
Socio-Demographic Characteristics
Of the initial sample of 398 participants, 385 completed the interview, yielding a response rate of 96.7%. Among these respondents, 199 (51.7%) were younger than 65 years, and nearly half were men (192; 49.9%). Regarding marital status, 229 (59.5%) were married, whereas 70 (18.2%) were widowed. Concerning educational attainment, the majority had completed secondary or preparatory education (95; 24.7%), whereas only 18 (4.7%) held a master’s degree or higher. With respect to economic status, 323 (83.9%) reported a monthly income greater than 15,000 Ethiopian birr (ETB). At the 2023 average exchange rate, 1 USD was equivalent to 54.7442 ETB. Additional details are presented in
Socio-demographic character of life style modification and associated factors among hypertension patients attending Eka kotobe hospital Addis Ababa, Ethiopia, 2023 (N:385)
| Variable categories | Frequency | Percent (%) | |
|---|---|---|---|
| Age categories | <65 YEARS | 205 | 53.2% |
| >= 65 years | 180 | 46.8% | |
| Sex | Male | 192 | 49.9% |
| Female | 193 | 50.1% | |
| Marital status | Single | 9 | 2.3% |
| Married | 229 | 59.5% | |
| Divorced | 68 | 17.7% | |
| Separated | 9 | 2.3% | |
| Widowed | 70 | 18.2% | |
| Educational status | Unable to write and read | 78 | 33% |
| Primary school (1-8) | 91 | 46.8% | |
| High school and preparatory school(9-12) | 95 | 20.3% | |
Life style and individual factors
Of the 385 respondents, 325 (84%) reported no comorbid conditions, whereas 53 (13.8%) reported a family history of hypertension. Overall, 356 (92.5%) of the participants possessed fundamental knowledge of lifestyle-modification strategies. Regarding treatment duration, 187 (46%) had received antihypertensive therapy for 2–5 years, and 180 (46.8%) had been diagnosed with hypertension within the same interval (see
Health profiles related Factors and individual factors of life style modification practice among hypertension patients attending Eka kotobe general hospital Addis Ababa, Ethiopia 2023(N:385)
| Variable categories | Frequency | Percent (%) | |
|---|---|---|---|
| Family history hypertension | Yes | 53 | 13.8% |
| No | 332 | 86.2% | |
| Comorbidity | Yes | 61 | 15.8% |
| No | 324 | 84.2% | |
| Duration of taking anti-hypertension drugs | <2year | 150 | 39% |
| 2_5year | 186 | 48.6% | |
| 6_10year | 48 | 12.5% | |
| Duration of diagnosis of hypertension | <2 year | 127 | 33% |
| 2_5 year | 80 | 46.8% | |
| >5 year | 78 | 20.3% | |
| Knowledge status life style modification | Good | 215 | 55.8% |
| Poor | 170 | 44.2% | |
Life style modification practice results
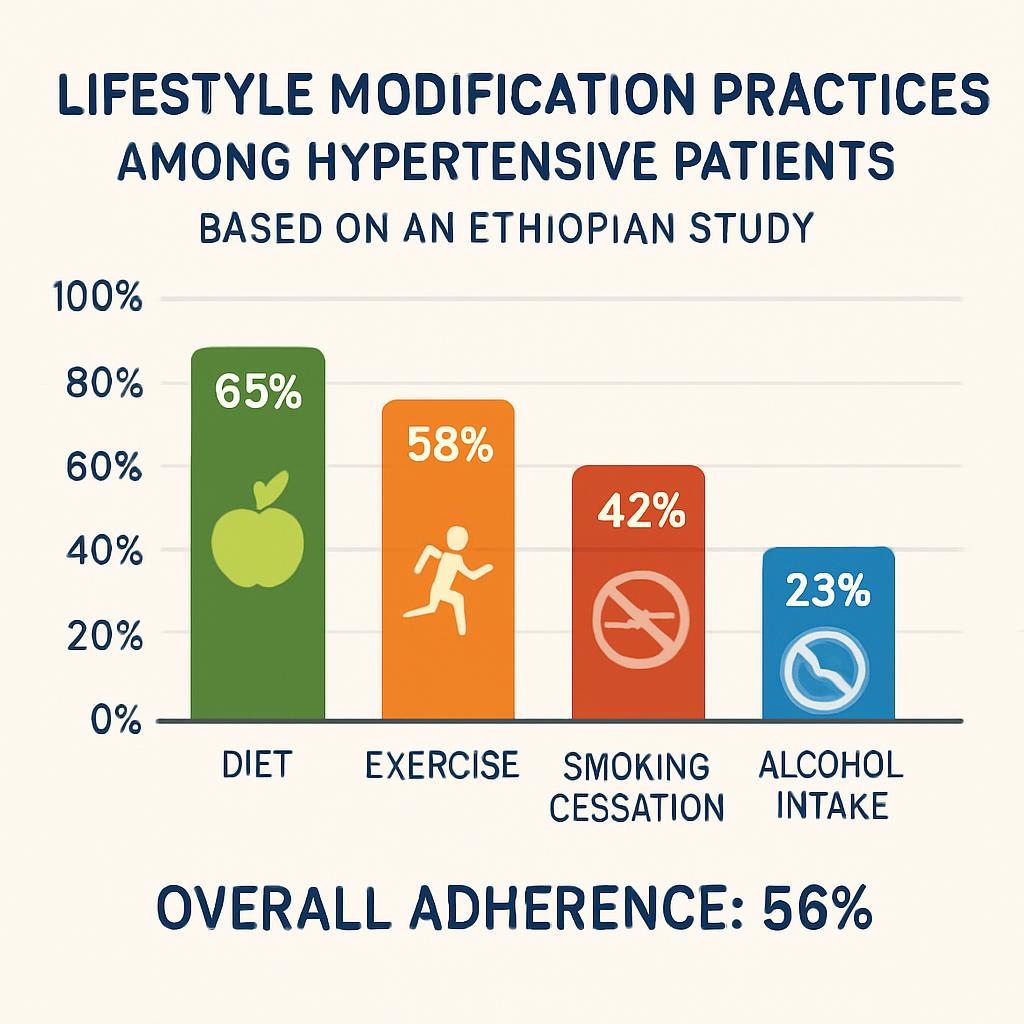
At Eka Kotebe General Hospital, 165 participants (42.9%) adhered to the recommended lifestyle modifications for hypertension management. Of these, 99 (25.7%) followed a low-salt diet. Only 23 % of the cohort engaged in ≥ 30 minutes of daily physical activity. Furthermore, 302 participants (78.4 %) were non-smokers, and 74 % had refrained from alcohol intake during the preceding seven days. Appropriate weight-management behaviors were documented in 156 participants (4.5 %). In addition, 84.9 % of respondents reported abstaining from khat chewing (see Figure 1).

Magnitude of life style modification practice among hypertension patients attending Eka kotobe general hospital Addis Ababa, Ethiopia, 2023(N: 385)
Factors Associated with Lifestyle Modification Practice
Binary logistic regression was employed to identify factors associated with lifestyle-modification practices among hypertensive patients. The independent variables comprised sociodemographic characteristics, level of knowledge, presence of comorbidities, duration of antihypertensive therapy, time since diagnosis, and family history of hypertension.
Variables with a p-value < 0.25 in the bivariate analysis were entered into the multivariable logistic-regression model. After adjustment for potential confounders, four variables remained statistically significant (p < 0.05): monthly income, age, comorbidity status, and knowledge level (
Predictor of life style modification practice among hypertension patients attending Eka kotobe general hospital Addis Ababa, Ethiopia 2023(N: 385)
| Identified factors | Category | Lifestyle of modification | COR (95%CI) | AOR (95%CI) | |
|---|---|---|---|---|---|
| Poor | Good | ||||
| Monthly Income the average | <= 1500 Birr | 43 | 19 | 1 | 1 |
| >1500 Birr | 177 | 146 | 1.867 (1.04, 3.34) | 2.48(1.3, 4.7)** | |
| Age categories | <65 YEARS | 129 | 70 | 1.924(1.28, 2.896) | 1.76(1.2, 3.1)** |
| >= 65 years | 91 | 95 | 1 | 1 | |
| Co-morbidity status | Had | 42 | 19 | 1.813(1.011, 3.253) | 2.2(1.13, 4.33)* |
| Had no | 178 | 149 | 1 | 1 | |
| Recommended lifestyle modification knowledge status | Had good knowledge | 140 | 75 | 2.1(1.392, 3.169) | 2.2(1.4,3.4)** |
| Had poor knowledge | 80 | 90 | 1 | 1 | |
Discussion
In this study, only a minority of patients with hypertension adhered to the recommended lifestyle modifications. Factors positively associated with adherence included higher income, younger age (<65 years), the presence of comorbidities, and adequate knowledge of lifestyle interventions. These findings suggest that targeted education and counseling, particularly for older adults and individuals with lower income, are essential. Hypertension is a major risk factor for cardiovascular disease and remains under-recognized, leading to substantial long-term morbidity, mortality, and economic burden 22. Enhancing patient awareness and systematically integrating lifestyle guidance into routine hypertension management may improve adherence and mitigate complications. Health professionals should prioritize patients at risk of poor lifestyle adherence and leverage comorbidity prevention visits as opportunities to reinforce healthy behaviors.
This study demonstrated that 43 % of hypertensive patients attending Eka Kotebe General Hospital practised appropriate lifestyle modifications. Factors independently associated with higher adherence included a higher monthly income, age < 65 years, the presence of comorbidities, and satisfactory knowledge of lifestyle-modification strategies.
The prevalence observed in the present study is consistent with a recent Ethiopian systematic review and meta-analysis, which documented a 41.5 % adherence rate to recommended lifestyle changes 24. By contrast, it is lower than the 50.8 % adherence reported among Chinese hypertensive patients 25, a difference that may reflect socio-economic and cultural heterogeneity. Within Ethiopia, the current figure is also lower than the 52.7 % reported in the northern region 6, possibly owing to discrepancies in sample size, study period, or regional health-care provision. Conversely, it exceeds the 23.6 % documented at Dessie Referral Hospital 23. Similarly, the 43 % adherence rate reported here surpasses the 26.9 % observed in Bishoftu (29) and the 33.3 % recorded at Mizan Tepi University Teaching Hospital 14, variations that could be explained by differences in screening instruments, sample sizes, study periods, and socio-economic circumstances.
In this study, monthly income, age, comorbidity status, and knowledge level emerged as significant predictors of adherence to lifestyle modification. Participants with higher income likely have increased access to reliable health information, nutritious food options, and facilities for physical activity. Those younger than 65 years were approximately twice as likely to follow the recommended lifestyle measures compared with individuals aged ≥ 65 years, consistent with findings from eastern Nigeria 26. This association may be attributable to greater health literacy and receptiveness to behavioural interventions in the younger cohort. Likewise, respondents with at least one comorbidity demonstrated a two-fold increase in adherence relative to those without comorbid illness, echoing results from Gondar, Ethiopia 11; more frequent interactions with healthcare providers may reinforce lifestyle advice in this group. Adequate knowledge also doubled the likelihood of practising lifestyle modification, affirming observations from Jimma University Teaching Hospital 27 and underscoring the central role of patient education 8. Despite these positive associations, overall adherence in the present study remained suboptimal. Taken together, higher income, younger age, presence of comorbidity, and good knowledge independently increased the odds of favourable lifestyle practices. These findings highlight the necessity for healthcare professionals to intensify targeted counselling and education—particularly for older adults, low-income populations, and individuals with limited knowledge—and to embed structured lifestyle guidance within routine hypertension care. Using comorbidity management as an entry point could further enhance adherence and improve patient outcomes. Overall, the data support an integrated, patient-centred, multimodal approach to hypertension management that involves clinicians, payers, and policymakers, thereby optimising health benefits and cost-effectiveness while accommodating local circumstances 21,22.
Despite the strengths conferred by a relatively large sample size and the employment of standardized assessment instruments, the present study exhibits several limitations. First, its cross-sectional design precludes the inference of causal relationships between lifestyle-modification behaviors and their associated determinants. Second, all information was obtained via self-reported responses, which are susceptible to social desirability bias and may have led participants to under-report poor practices or over-state adherence. Finally, the application of systematic sampling restricted to patients attending follow-up during the study period may have introduced selection bias, as this sample might not represent all hypertensive patients in the broader community, thereby limiting the external validity of the findings outside the hospital setting.
Conclusion
This study found that the overall prevalence of adequate lifestyle-modification practices among hypertensive patients was low. Higher odds of good practice were associated with greater monthly income, age < 65 years, the presence of co-morbidities, and good knowledge of lifestyle modification. Accordingly, healthcare providers should intensify counselling on lifestyle changes, regularly assess patients’ knowledge, and integrate co-morbidity prevention into their interventions. Particular attention is warranted for patients at risk of poor adherence. Patients must be educated about the pivotal role of lifestyle modification in hypertension management. Health professionals and institutions should strengthen awareness campaigns, motivate patients, and provide verbal reinforcement to enhance knowledge and sustain behavioural change. Special counselling for widowed patients and opportunities for peer learning from individuals who demonstrate good practice are recommended. The identified determinants—advanced age (> 65 years), co-morbidities, and inadequate knowledge—underscore an urgent need for multicomponent interventions tailored to resource-limited settings.
Abbreviations
AOR: Adjusted Odds Ratio; BP: Blood Pressure; CI: Confidence Interval; CVD: Cardiovascular Disease; DASH: Dietary Approach to Stop Hypertension; DM: Diabetes Mellitus; ETB: Ethiopian Birr; H-SCALE: Hypertension Self-Care Activity Level Effects; HTN: Hypertension; JNC 7: Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; LF: Lifestyle; LMICs: Low- and Middle-Income Countries; LSM: Lifestyle Modification; LSMs: Lifestyle Modifications; NCD: Non-Communicable Disease; NCDs: Non-Communicable Diseases; OPD: Outpatient Department; OR: Odds Ratio; SPSS: Statistical Package for the Social Sciences; SSA: Sub-Saharan Africa; VIF: Variance Inflation Factor; WHO: World Health Organization.
Ethical Consideration
This Study Confirmed that all Methods were carried out in accordance with relevant Guidelines and Regulations, all experimental protocols were approved and confirming that participant confidentiality and anonymity were strictly maintained throughout the study. Permission letter was obtained from Eka kotobe general hospital from research committee. Information sheet was prepared and read to all eligible participants of the study. Write informed consent will receive from all participants .All participants was informed the purpose of the study and their participation is on voluntary basis. Name of the participant was omitted from the questionnaire. Confidentiality and privacy were ensured at all levels throughout the study by keeping the data and records in a safe place.
Consent to publish
Not applicable
Availability of data and materials
The datasets used in this study are available from the corresponding author upon reasonable request.
Competing interests
Authors declared that they have no competing interest
Funding
Funding for this study was obtained from the University. The University had no role in the design of the study, collection, analysis, or interpretation of data.
Author Contributions
KMH contributed to the conception, design, and conduct of the study; analysed and interpreted the data; prepared the manuscript; contributed to the conception, design, and conduct of the study; analysed and interpreted the data; and prepared the manuscript.
MEY,EMA and DBD contributed to the design and conduct of the study, analyzed and interpreted the data, and prepared the manuscript. All the authors have read and approved the final manuscript.
Acknowledgment
Our special thanks are forwarded to the data collectors, supervisors, and hospital administrators for their devoted time and unreserved participation. Finally, the study participants, data collectors, and Eka kotobe general hospital Research Ethical

